Kyle Harper’s new book, Plagues Upon the Earth: Disease and the Course of Human History, shows that the story of disease is entangled with the history of slavery, colonialism, and capitalism. In this excerpt, he explores the relationship between poverty and health.
Editor’s note: The current debate in economics seems to lack a historical perspective. To try to address this deficiency, we decided to launch a Sunday column on ProMarket focusing on the historical dimension of economic ideas. You can read all of the pieces in the series here.
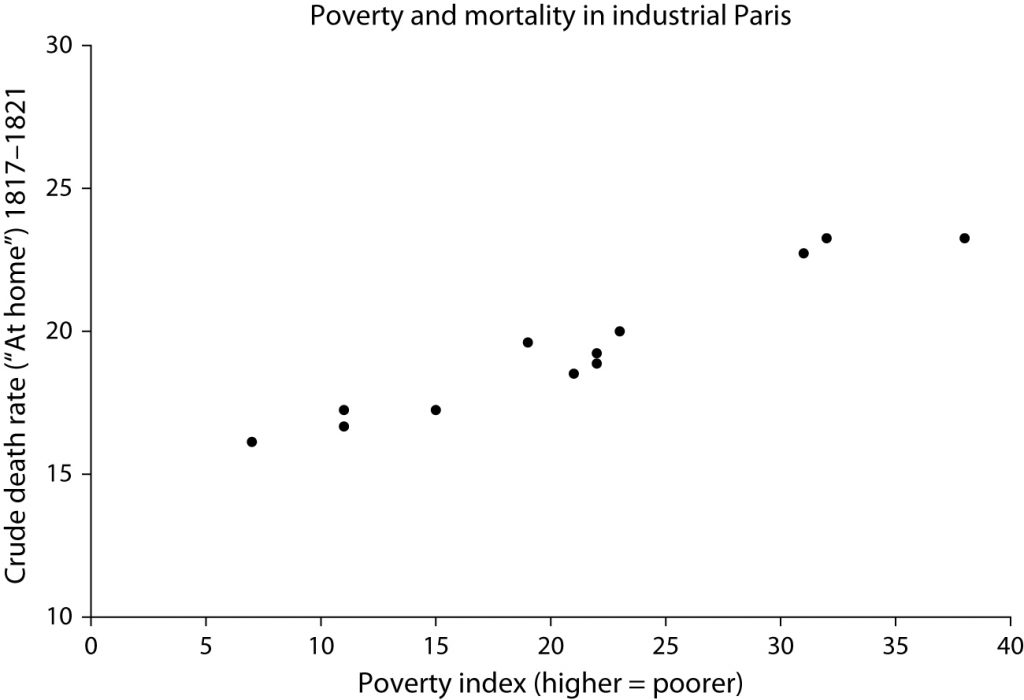
In the 1820s, the French intellectual Louis-René Villermé set out to answer definitively the question of whether the rich lived longer than the poor. Villermé had served as an army surgeon for ten years under Napoleon and then earned his doctorate in medicine. He had the means to set up as an independent intellectual in Paris, and he devoted himself to the study of population health. To test whether social status influenced mortality, Villermé did something on the cutting edge of social thought: he used statistics. Drawing from new sources of public data, he conducted an ingenious analysis of mortality in Paris. He looked at mortality rates in every district (arrondissement) of the city, and then explored a range of variables for each district in search of associations with the mortality rate. One clearly stuck out: a poverty index that he had created for each district. The parts of Paris with the highest proportion of poor households also suffered the highest death rates (see figure 10.9).
These results might seem unsurprising to us. Today, people who enjoy higher socioeconomic status also enjoy longer and healthier lives thanks to greater access to medical care, lifestyle differences, and lower physiological stress, among other things. But in the past, social inequities did not necessarily translate into health inequities. The relationship between social status and health outcomes is a product of history. When and how did wealth come to entail greater health?
It is hard to say. The evidence is contradictory. The issue is complicated first and foremost by the urban mortality penalty. Even though by 1800 improvements in urban health had been achieved, the countryside was still far more salubrious than the city. In 1811, people in urban England had life expectancies ten years shorter than those of their rural counterparts; half a century later, the gap was seven years; in 1911, it was reduced to three. Because elites tended to live in towns, their health was concomitantly endangered. Moreover, correlations between status and health are sensitive to how “elites” are defined, especially given the changing nature of social relations in a period that fostered the rapid rise of a middle class. Nevertheless, behind the noise, there are signals of an epochal shift in the history of health inequality, as for the first time social and biological status came to mirror one another consistently.
In 1967, the social scientist Aaron Antonovsky proposed that class differences in life expectancy could be divided into three periods. During the first, which lasted until about 1650, there were not class gradients in mortality. From about 1650 to about 1850, the class gap widened, and in the period since, it has narrowed. The schema remains useful. Before the early health transition, when infectious disease was effectively uncontrollable, high social status had a negligible, variable, and at times even inverse relationship to health status. The early health transition then created health inequities, as elites were able to convert social advantage to longer life. Later, the more sweeping transition of the late 1800s dispersed the benefits of scientific and economic progress more widely, narrowing the gap in life expectancy but never completely closing it. Most of the early evidence for elite life expectancy comes from the top echelons of society. Infectious disease was not a respecter of persons. The Roman emperors, for example, had poor lifespan prospects due to the hazardous disease environment of the ancient Mediterranean.
A thorough study of European nobility since AD 1000 found that life expectancy fluctuated, suffering in times of war and plague. It was not unusual for aristocrats to experience higher mortality than average people, especially people who lived in the countryside. A famous study of the British peerage shows that its members suffered higher-than-average mortality rates until the eighteenth century.
But there must often have been times when higher social status improved the prospects of survival. Even in premodern times, the affluent fared better during periods of crisis. Malthusian theory predicts that the “positive check” will affect the destitute, whose conditions fall below the minimum level required for subsistence. The great famines of early modern history no doubt carried off the poor in disproportionate numbers. In the London plagues of the seventeenth century, the poorest parishes in the metropolis suffered higher mortality than the wealthier, central parishes. A careful study of the population of Geneva, going back to 1625, shows that there were already gaps between the well-to-do and the poor, and that the lower classes benefited from a general increase in life expectancy during the eighteenth century. In some contexts, therefore, social advantage surely led to longer lifespans even before the early health transition.
What happened between about 1750 and 1850, then, was the formation of persistent social cleavages in health. Elite and bourgeois life expectancy rose, while the poor struggled to climb at the same pace. The British royal family, a small sample, turned a corner after 1700, with much greater chances of survival from the eighteenth century on. But they were ahead of the curve. Adult survivorship among elites only surpassed that of the lower classes around the middle of the century, and even then the pattern is clouded until the early nineteenth century. Other data sets corroborate that over the course of the eighteenth century, even middling elites—merchants and professionals—were able to achieve lower infant and child mortality rates than the working classes.
Early public health reformers started to explore the complex links between health inequities and social inequities. The German physician Johann Peter Frank published the first volume of his monumental Complete System of Medical Policy in 1779. It was a landmark in “the history of thought on the social relations of health and disease.” When Frank lectured in 1790 on “the people’s misery” as the “mother of diseases,” he observed the multifaceted connections between class and the experience of disease: “Every social group has its own type of health and diseases, determined by the mode of living. They are different for the courtiers and noblemen, for the soldiers and scholars. The artisans have various diseases peculiar to them, some of which have been specially investigated by physicians. The diseases caused by the poverty of the people and by the lack of all goods of life, however, are so exceedingly numerous that in a brief address they can be discussed only in outline.”
“Villermé was right: industrialization had left the poor more susceptible to infectious disease and early death than their bourgeois counterparts.”
By the early nineteenth century, the resulting gap was visible to the naked eye. The first wave of industrialization was brutal for the working poor. As de Tocqueville observed of 1830s Manchester, “From this foul drain the greatest stream of human industry flows out to fertilize the whole world. From this filthy sewer pure gold flows. Here humanity attains its most complete development and its most brutish; here civilization works its miracles, and here civilized man is turned back almost into a savage.” This was the stark inequity that inspired sanitary reformers like Edwin Chadwick, whose Report on the Sanitary Condition of the Labouring Population of Great Britain appeared in 1842. In sum, in the words of historian Peter Razzell, “Poverty became more important in shaping mortality in the nineteenth century through its association with disease environment. With the development of large cities and industrial areas, social classes became increasingly geographically segregated, leading to an association of poverty with ‘the slum.’”
Villermé was right: industrialization had left the poor more susceptible to infectious disease and early death than their bourgeois counterparts. There is a silver lining, though, in that these inequities galvanized the public health movement and created the political energy for reform. From Frank to Villermé to Chadwick, the political energy of health reform took shape in different guises across western Europe and the United States. The shorter and unhealthier lives of the poor seemed an affront to justice and a problem that could be remedied. Villermé’s methods—using statistical investigation to understand the range of influences on health outcomes—pointed toward the future. Villermé’s career reminds us that the golden age of public health reform has its roots in the preceding generations, in the ideas and methods of the Enlightenment and in the negative feedbacks of industrial growth.
Excerpted from Plagues Upon The Earth: Disease and the Course of Human History by Kyle Harper. Copyright © 2021 by Kyle Harper. Reprinted by permission of Princeton University Press.